We encourage our patient and public members to share their experiences about their condition and their research involvement experiences on this page.
Royce Biomedical Materials Event
24th April 2019
“A highly informative and interesting presentation given by Professor Sarah Cartmel about the interaction between the various universities involved and the Royce Institute at Manchester. The facilities and technology that is available for in-house researchers, PhD Students and MedTech Companies and available for them to have access to was quite mind blowing. Sarah gave some very useful future ideas of where this bio-medical materials research may be used.
A specific one was the repair of tendons and worn out cartilage replacement.
Some of the research equipment referred to which was of world class quality was I am afraid over my head but I did learn much about the way bio-medical technology was going and this meeting gave me some useful knowledge to support my role of PPI for the NIHR Medical Technology Cooperative.”
Philip (socks) Bell



27th March 2019
I attended the EPSRC Information Day and below is a brief report and some photos.
The venue was the delightful Birmingham Botanical Gardens – even the peacocks were interested and the weather was fabulous enabling us to sit outside in the breaks.
The event was well subscribed with not one spare seat available. It was a delightful mix of all levels of health and social care researchers from the highly technical imaging and robotic scientists to computing and data analysts with a mixture of patient facing health professionals – and of course there was me! the only PPI person there. There was no seating plan and delegates just sat at a table wherever. Nonetheless I was treated as a total equal and my comments and opinions were avidly listened to and genuinely made to feel part of the team working on our table.
The discussions were not overly technical but conceptual and easily within the understanding of a member of the general public with some experience and knowledge of the NHS. I would thoroughly recommend that everybody attends these events as they are both enjoyable and informative.
Colour of socks are optional but believe me there were some brighter ones than mine there…..
Philip Bell





22nd August 2017
 Roger Llewellyn thought his days as an active sportsman were numbered when his large-intestine was removed to treat his ulcerative colitis. Five years on from his surgery, Roger describes how a few stumbling steps led to a triathlon, a treetop adventure and a tandem skydive.
Roger Llewellyn thought his days as an active sportsman were numbered when his large-intestine was removed to treat his ulcerative colitis. Five years on from his surgery, Roger describes how a few stumbling steps led to a triathlon, a treetop adventure and a tandem skydive.
After trying various drugs and treatments for his ulcerative colitis, Roger was referred to Professor David Jayne, Clinical Director for the Leeds Colorectal Therapies HTC and Professor of Surgery at the University of Leeds and Leeds Teaching Hospitals NHS Trust, who conducted surgery to remove his large intestine.
The reality of life after surgery was difficult, with a challenging period of adjustment. “After my operation, for a time I just stopped,” says Roger. “There were a lot of things I wanted to do in my life, but I thought I couldn’t.”
Things changed when Roger’s brother-in-law mentioned completing a triathlon in late 2016. Excited by the idea, Roger entered the Blenheim Triathlon – but training proved tough.
“I hadn’t done any sport in over five years, and I had very little strength.” Roger says, describing his first attempt at jogging after taking part in a 5km Park Run. “I started running, but after 100 metres I had to stop and walk.” He wasn’t deterred, and went on to complete the course in a creditable time.
Inspired, that first run was the start of an intense period of training, with Roger swimming and jogging three times a week and fitting in a cycle ride whenever possible. In June he completed the Blenheim Triathlon, swimming 750m swim, cycling 20km and running 5.6km. He enjoyed it so much, he completed the Leeds Triathlon a week later. The physical challenge was hard, but it has helped in other ways too. “It got me out of a mental hole,” he says.
Since completing the triathlon Roger has run through the tree tops at an adventure park and completed a tandem skydive, leaping from a plane at 15,000 feet.
A supportive family mean Roger hasn’t had to face the condition alone – and there are many more adventures to come, with Roger and his partner planning a trip to the Arctic Circle. “You have to be brave to do things, but you also need to be practical and plan ahead,” he says.
When asked what message he would give to anyone concerned about living with ulcerative colitis or worried about surgery, Roger is upbeat: “It can be a difficult and painful condition to live with, but it doesn’t have to define you. It should never stop you doing the things you want to.”
7th November 2018
 Treatment for bowel cancer usually involves surgery. A period of recovery after surgery is normal, but this can be an anxious time. There are many different aspects of recovery. Some include the control of pain, rebuilding of a normal diet, regaining good energy levels, and being able to use the toilet comfortably. This process starts in hospital and may continue for several weeks or even months at home.
Treatment for bowel cancer usually involves surgery. A period of recovery after surgery is normal, but this can be an anxious time. There are many different aspects of recovery. Some include the control of pain, rebuilding of a normal diet, regaining good energy levels, and being able to use the toilet comfortably. This process starts in hospital and may continue for several weeks or even months at home.
Information about recovery can help to alleviate anxiety. This may be provided as a printed leaflet, an internet resource, or a “recovery workshop” before the day of surgery. Unfortunately, the availability, format, and quality of this information can be rather variable. Researchers at the University of Leeds are interested in how information can be improved to make it more useful and accessible to everybody. They wanted to find out more from patients who have had bowel surgery in the past.
Leeds focus group
Eleven people from across the United Kingdom took part in a focus group. This was held in Leeds at the NIHR Surgical MedTech Co-operative National Meeting. The focus group had two aims. The first was to find out what aspects of recovery after surgery are most important to patients. This will help researchers to design the content of future information resources. The second aim was to explore how and when the information should be provided. This will help to avoid situations where patients feel overburdened.
The focus group ignited lively discussion from participants who had very diverse experiences. It was fantastic to hear real-life perspectives from people who were enthusiastic about improving care for others in the future. Both positive and negative insights were shared and key areas for improvement were identified. It became clear that collaboration between patients, healthcare professionals, and information design specialists would be essential for designing new and effective resources in the future.
Outcomes
Following the focus group, the researchers will produce a summary of results. This will be used to decide how current information resources about recovery can be improved. The results will be published in a scientific journal and sent directly to people who took part in the focus group. The researchers are particularly interested in how patients and the public can stay involved in future stages of this work. Their insights and experiences will be essential to make sure future information resources are relevant to patients from all backgrounds.
Eventual benefits
Information given to patients about their recovery must be fit for purpose. The researchers hope that improving this information will help relieve some anxiety and improve patients’ experiences throughout their recovery. This research alone will not achieve this ultimate aim, but it will help to guide the researchers in the right direction.
The focus group was made possible by support from Bowel Cancer UK and the NIHR Surgical MedTech Co-operative. The researchers are most grateful for their assistance. They are also thankful to the participants who offered their valuable time to make this research possible.
Authors:
Stephen Chapman, Academic Clinical Fellow & Surgical Trainee, University of Leeds, Email: S.Chapman@leeds.ac.uk; Twitter: @SJ_Chapman
Carolyn Czoski-Murray, Senior Research Fellow in Applied Health Research, University of Leeds
FU = Stands for Faecal Urgency. Which is the medical definition for “struggles to hold a poo in” and “when one drops into the chamber, you had better have your shit together (get it) in knowing where you can drop it off“.
Who’s the author:
I’m a 38 year old man with two kids and a very glamorous wife.
That’s right, I am a Male.
Yes, a MALE…!!!
Men don’t tend to talk about this stuff, so I thought I would break the taboo and get typing….if I can help one person then all this has been worth it.
Thank you Andrew for allowing the Surgical MIC to share your story
If you weren’t able to attend the sessions, these write ups will provide an overview of the discussions and the outputs from the event. The team at the Centre for Engagement & Dissemination are now reviewing all of the comments and recommendations generated and developing their next steps for action and how we’ll continue the conversation.
– Workshop 1: Ideas generation
– Workshop 2: Refining and prioritising our ideas
– Workshop 3: Working together to achieve impact
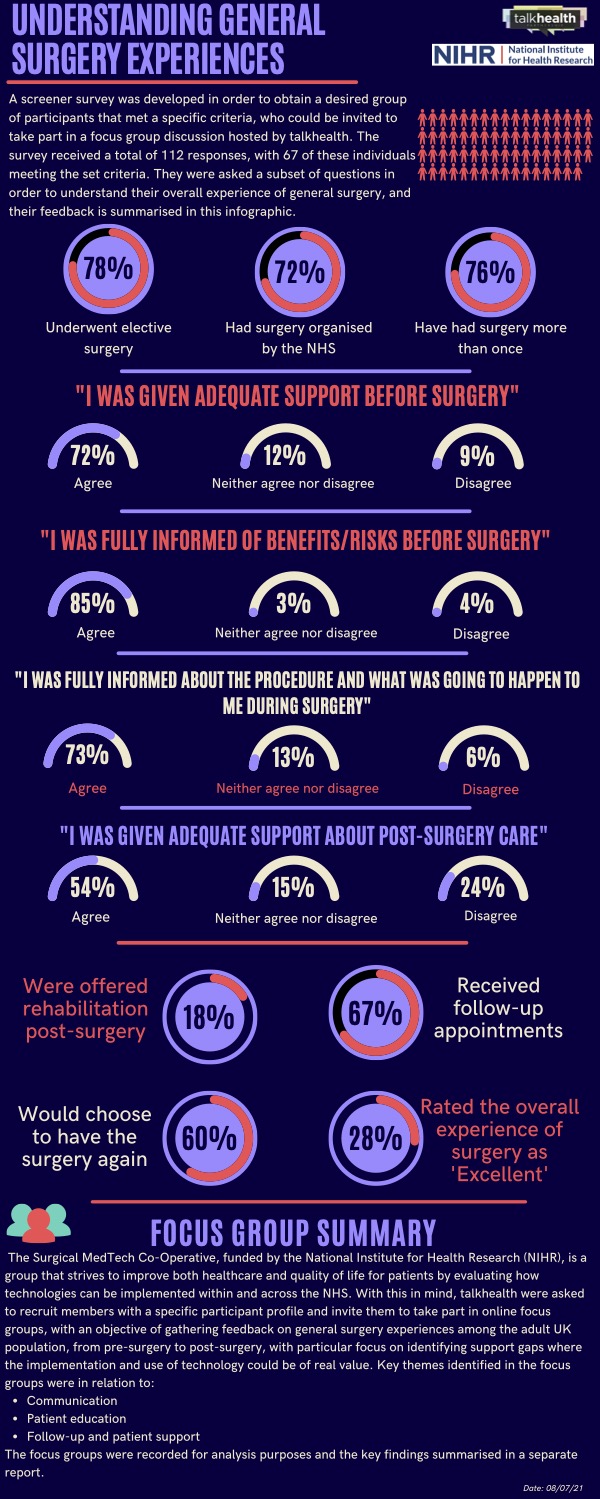
Two online focus groups were conducted with the aim of better understanding the experience of general surgery, from pre to post, highlighting and exploring any support gaps. The focus groups were also used as an opportunity to identify how technology could be used within areas that need improvement and whether technology played a part in the participants’ experiences of surgery.